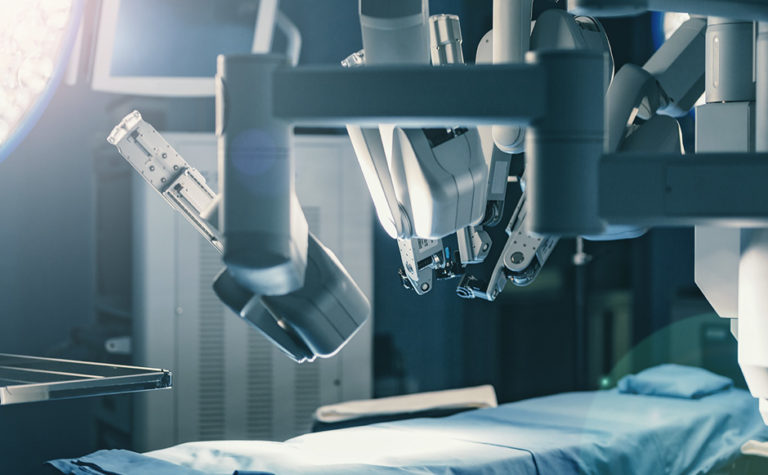
Robotic Surgery
Robotic surgery is a type of minimally invasive surgery that allows surgeons to perform complex surgical procedures through small incisions in the abdomen. It is a lot like laparoscopic surgery but the robotic instruments are smaller and are manipulated via robotic translation of human movements. What this means is the surgeon is able to perform surgery with more precision, flexibility and control than other forms of surgery such as laparoscopy. Patients tend to have less pain and stay fewer days in the hospital when compared to surgical procedures that are done through large abdominal incisions. Complication rates are similar to other forms of surgery when the robotic surgery is performed by an experienced robotic surgeon.
When a surgeon performs robotic surgery, he/she sits at a console (similar to a virtual reality video game controller) where there are hand motion sensors and an eyepiece he/she looks through. The motion sensors translate all of the surgeon’s hand and finger motions into the small robotic instruments that work inside the abdomen to perform the surgical maneuvers. The eyepiece allows the surgeon to see into the abdomen 3-dimensionally and in high definition. The abdomen is filled with gas (usually carbon dioxide) to allow improved visualization of the surgical site. The robotic instruments have near-360 degree movement, very similar to human wrists.
Many surgical procedures have traditionally been performed through large abdominal incisions based upon the complexity of the surgery. Robotic surgery, however, allows surgeons to perform these procedures through small, less painful incisions. Robotic surgery is commonly used for gynecologic procedures, but is also used for urologic, thoracic and colorectal procedures.
Urogynecologic procedures performed robotically include hysterectomy, uterosacral ligament suspension and sacrocolpopexy. Urogynecologists have extensive training in these surgical procedures. Your urogynecologist can determine if you are a candidate for any of these procedures.
Urogynecology is a relatively new subspecialty of obstetrics and gynecology. It has grown out of need. Urogynecologists focus on the care of women with bladder issues and symptomatic pelvic floor relaxation.
For time immortal, there has been a need for therapies to treat the problems women face that are related to childbirth, aging and the forces of gravity. When women go through pregnancy and vaginal delivery, the organs of the pelvis are stretched and rarely return to their pre-baby state. These effects are amplified by age, a genetic predisposition and other medical conditions such as diabetes. When the uterus and vagina lose their normal support, they begin to fall. They can even fall outside of the vaginal opening. This phenomenon is called pelvic floor relaxation or prolapse. There are several different types of prolapse. [link to types of prolapse] For years, the best treatments doctors had to offer for these issues were exercises, open abdominal surgeries with large incisions and difficult recoveries or the use of pessaries, which are devices that must be worn constantly to physically push the organs back up into the vagina and hold them in place.
Enter the DaVinci Surgical Robot
Surgical robots were originally developed by the military with the idea that a surgeon could operate on a wounded soldier from a remote location, sort of like flying a drone. What has evolved is totally different. The robots are now used by surgeons sitting at a console in the same operating room where the patient is. The advantage the robots offer is that surgeons can do very delicate surgeries inside the abdomen through very small poke holes rather than through large incisions. The result of all that is that the patients can have less blood loss, less post-operative pain, and require fewer days in the hospital. In fact, the surgical robot actually makes some surgeries much more practical than their open counterparts have always been. Specifically speaking, the gold-standard surgery for uterine prolapse is the sacrocolpopexy, which has traditionally been performed through a large incision on the abdomen.
1. Robotic Sacrocolpopexy
The Robotic Sacrocolpopexy is performed mostly by urogynecologists. It is done in conjunction with a robotic hysterectomy in women with utero-vaginal prolapse. It is also done alone in women who have previously had a hysterectomy and now have vaginal vault prolapse. [link to types of prolapse] In a Robotic Sacrocolpopexy, from inside the abdomen, a Y-shaped piece of flat surgical mesh is used. The arms of the “Y” are sewn to the front and back of the vagina respectively and the stem of the “Y” is sewn to a ligament on the inside of the sacrum (lower part of the spine attached to the pelvic bones.) This procedure lifts the vagina back into the pelvis and securely holds it there. This surgery has a high success rate, higher than most other prolapse surgeries, making it the gold standard surgery for the treatment of uterovaginal or vaginal vault prolapse. When indicated, a procedure for urinary incontinence can be done at the time of a sacrocolpopexy. [link to types of urinary incontinence]
Benefits:
The primary benefit of this surgery is obvious. It is that the patient’s pelvic organs are no longer falling out of the vaginal opening.
- Improved Comfort: The women who have had these procedures report that they are more comfortable both mentally and physically when not having to deal with the constant vaginal pressure and discomfort.
- Peace of Mind: This obviously goes with the above topic, but women are happier after these surgeries, because they no longer have the anguish that goes along with constant worry about feeling less feminine, poor sexual performance, and embarrassment.
- Improved Urination: Another less obvious benefit is improvement in urination. By pulling the vagina back into the pelvis, the urethra (the tube from the bladder to the outside) is pulled back into a more normal alignment allowing more normal urine flow, without obstruction. This can improve the bladder’s ability to empty and reduce the risk of urinary tract infection.
- Improved sexual intercourse is not guaranteed, but is often reported by patients. It only makes sense that if the vagina is held firmly back inside the pelvis instead of falling out, vaginal intercourse would be easier and more gratifying for all parties involved. Many patients report this sort of result. However, in a small percentage of cases, the implanted mesh can erode through the vaginal wall making intercourse uncomfortable for male sex partners. Also, any prolapse repair procedure, not just sacrocolpopexies, can lead to discomfort with intercourse, but fortunately, these problems are the exception rather than the rule.
2. Robotic Uterosacral Ligament Suspension
Another surgical option for uterovaginal prolapse that can be done robotically is a uterosacral ligament suspension. In this surgery, the surgeon ties the upper part of the vagina to a pair of ligaments in the pelvis called the uterosacral ligaments. These ligaments lie on either side of the lower part of the sacrum and are in part responsible for suspension of the top of the vagina. This is done with suture. No surgical mesh is used. It has the same goals and benefits as the Sacrocolpopexy. The main difference is that many studies have found the Uterosacral Ligament Suspension has a slightly lower long term success rate when compared to the sacrocolpopexy. One of the benefits of this procedure is that since there is no mesh used, mesh erosion is never an issue.
Surgeries Often Performed in Conjunction with Robotic Lift Surgeries:
- Anterior Colporrhaphy
- Posterior Colporrhaphy
- Urethral Sling
Other surgeries are often performed together with one of the above procedures. If the patient has a weak front vaginal wall and her bladder is bulging into her vagina, this is called a Cystocele. The surgery for this is called an Anterior Colporrhaphy (commonly known as an Anterior Repair). If her back/posterior vaginal wall is weak and the rectum is bulging into her vagina, this is called a rectocele. For this, the patient might need a Posterior Colporrhaphy (Posterior Repair). If the woman leaks urine when she coughs or laughs, it is called Stress Urinary Incontinence. The most common surgery for that is a Urethral Sling procedure to help prevent urine leakage.
The sub-specialty of Urogynecology has grown rapidly since the introduction of the surgical robot, but not all Urogynecologists are firm believers in robotic surgery. Some of these doctors still prefer open procedures because that is what they have experience doing.
A Guide for Men
This is where we thought we would put “How to Take Care of Her When She Gets Home,” but let’s face it. The guys want to know…
“When can we have sex?”
The answer to that question can vary depending on the situation, including what surgery or surgeries are done. Usually, it is something like six weeks, but may be longer, depending on the woman’s comfort. Another major factor affecting this answer is whether or not she had other procedures done along with lifting her pelvic organs, especially the Anterior and/or Posterior Colporrhaphy (Anterior and/or Posterior Repair). You will have to ask her doctor this question to know for sure.
Will sex be more gratifying for her and for me?
Improved sexual intercourse is not guaranteed, but is often reported by patients and partners. It only makes sense that if the vagina is held firmly back inside the pelvis instead of falling out, vaginal intercourse would be easier and more gratifying for all parties involved.
How to Care for Her When She Comes Home.
When the patient comes home, she will need some help. The most important thing is for her to not lift heavy items. The action of lifting heavy items will cause an increase in pressure in her abdomen (belly), which will then cause an increase in force downward on her vagina, thus increasing the risk of the repair failing. So, someone else should do all the household chores she usually does, for at least six weeks. Any chores that require lifting more than ten pounds should be done by someone else for at least six weeks.
When can she go back to work?
That depends on the type of work she does and what type of procedure she had. If she sits at a desk, she may be able to return to work in as little as two weeks. If she does heavy construction, it could be as long as ten weeks. You would need to discuss this with your doctor.
